SuperChickens?
In this final part of my series on antibiotic resistance, I want to discuss the use of antimicrobials in the food supply. If you need to review other areas of antibiotic resistance, check out “Discussing the Disappearing Miracle” (a lesson in what antibiotic resistance is and is not), “Quitting When You’re Not Really Ahead“ (how people accidentally contribute to antibiotic resistance), and “No, the Z-Pack Won’t Treat The Flu” (how overprescription of antibiotics contributes to resistance). In this article, I’ll focus on how antibiotics are used in the growth of animals destined for consumption, what that does in terms of producing resistance, and what we can do in response.
I know the article is called “SuperChickens?”, but I actually want to start by talking turkey. If you live in the United States, you’ve likely seen the president pardoning a turkey on Thanksgiving Day. This is an old tradition - you can see a photograph of Kennedy pardoning a turkey next to a similar photo of Obama doing the same thing 50 years later (1). What’s remarkable in this photo is the difference in the two birds. Kennedy’s turkey is much closer in size to wild turkeys (2), which usually weigh between 7.6 kg (toms) and 4.26 kg (hens), maxing out at 16.85kg (3). In comparison, the turkeys that grace most tables average 13.5 kg, maxing out at 39 kg (4). Wild turkeys are half the mass of modern, domesticated turkeys (2). Nor did that change happen by accident.
Until the 1950s, most turkeys were similar to the wild birds. However, with the arrival of antibiotics, the average size of the bird began to change. While this was initially done through selective breeding, the demand for meat incentivized not only breeding for size, but also speed from egg to adult. The demand for a bigger bird faster drove competition. When it was discovered that antibiotic use increased the growth rate of chicks in 1948 (chicks given antibiotics grew larger, faster, than those not given antimicrobials), it helped create a new market for the new drugs (5). Since faster growth resulting in bigger birds was the desired outcome, the animals’ feed was soon supplemented with antibiotics.
I know what you’re wondering - who even thought that feeding antibiotics to chickens was a good or necessary idea? It turns out that the introduction of antibiotics was an accident. Researchers were studying other ways to supplement growth, focusing on vitamin B12 (which includes cobalt, a trace metal important for red blood cell development, neurological function, and DNA synthesis) (6). The researchers were looking for different sources of B12, and one easily available source used was the cellular remains of Streptomyces auerofaciens (5). These bacteria were used to develop the tetracycline antibiotic aureomycin, and the cellular remains were what was left when the antibiotics were extracted from the bacteria. They used it because it was an amazing source of the vitamin for a very low cost - it was waste from another process already being done. Another source of B12 was beef liver. Researchers discovered that the chicks given bacterial remains grew 24% faster than the chicks given liver. While it wasn’t initially clear that the antibiotic residue in the cellular remains caused the growth, the vitamin was eventually ruled out as the cause of improved growth (5).
Suddenly, agriculture had an easy way to improve their product - they could grow animals faster, larger, which meant they could use less feed - the sooner an animal was an adult, the sooner it could be sent to market. Since the initial doses of antibiotics were accidental and very low, antibiotics for growth promotion also use very low doses. As a result, the bacterial population in animals are exposed to the drugs used to treat an infection in a sick animal, but over the entire course of their life. This establishes an excellent environment for the bacteria to adapt to the drug and become resistant to it.
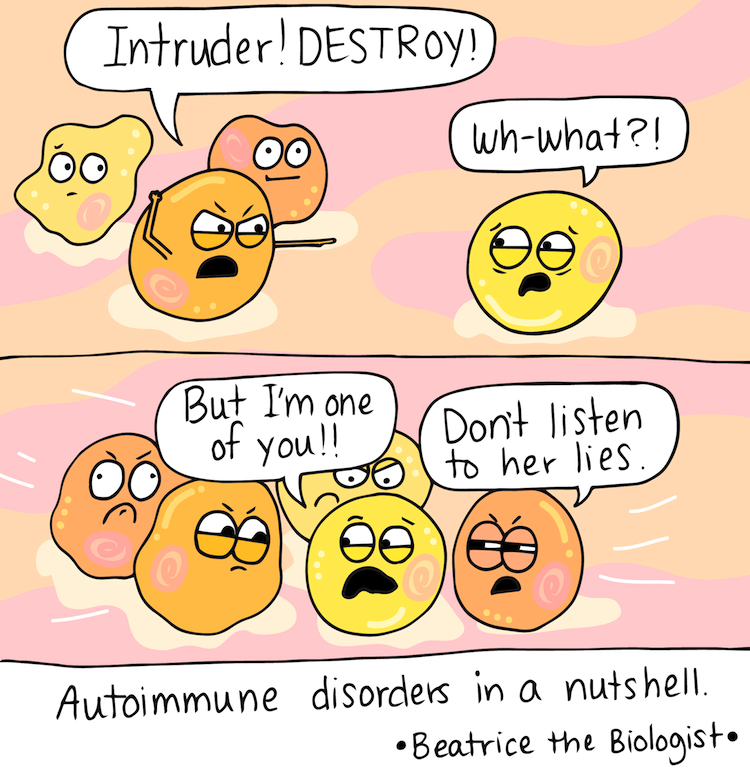
See, resistance occurs when a bacteria is exposed to a drug, but not all of the bacteria are killed by the drug. The weakest bacteria die off, leaving those not actually susceptible. During clinical dosing of antibiotics (when used to treat an infection), high doses are used over a short course. This makes it more difficult for the bacteria to adapt. The high dose is more likely to eliminate more of the bacteria, and the short course, or amount of time involved actually taking the medication, means that any resistant bacteria don’t remain exposed to the drug long-term. That gives our rapidly multiplying bacterial population no opportunity to select for resistance. Instead, as the resistant bugs die off, random chance re-enters the evolutionary picture - there’s nothing present to make the resistant bugs more likely to survive and reproduce, so there’s no benefit to resistance.
But when the exposure is low, more of the bacteria survive, giving a larger population the ability to adapt (versus the much smaller population of resistant bacteria that exist after the rest are killed off). What makes this worse is when that exposure occurs over a long period of time. The benefit of remaining resistant continues, which ensures that the larger population is more likely to retain resistance. Random chance is thus limited when mutations occur - the pressure to remain resistant persists within the bacterial community, producing more resistant bacteria in greater numbers.
Growth promotion isn't the only use for antibiotics in agriculture. When one or more animals is ill, or when stress is high within the population (such as weaning the young or transporting them), farmers use antibiotics to prevent illness in the entire community. This preventative use makes use of higher doses than those used for growth promotion, but still lower than needed to treat active infection. This subclinical dosing (lower than needed to treat an infection) in both cases increases the exposure of bacteria to the same drugs used to treat disease in both animals and humans. While this preventative use need not be used over an extended period time, not all farms as judicious as they could be in their use. However, this use of antibiotics creates a similar selection pressure on the bacterial populations within the animal - it's still high enough to eliminate the most susceptible bacteria, but because no active infection is present, the animals' immune system never activates to eliminate the remaining, resistant population. Worse, because this dose is higher than the one used for growth promotion, the percentage of the population that remains is made up of mostly resistant bacteria (as opposed to resistant and non-susceptible bacteria that remain with the very low doses involved in growth promotion).
The least controversial use of antibiotics in food production occurs when an animal is actually ill. In these cases, sick animals are given clinical doses of antibiotics, just as the rest of us are. Since the animal is reliant on another to dose them, either in feed, water, or via injection, the risk of forgetting a dose is reduced. Some farmers do this by adding the medication to the water supply, but if it is only supplied to the infected animals, the risk of resistance drops. Since it’s illegal (and unprofitable) to sell sick animals, very few object to clinical uses in these settings (although some farms ban the use of all antibiotics, or won’t sell animals that required treatment).
OK, so animals can develop resistant bacteria just like people do. You may be asking yourself why that matters. We can’t give animals cold medicine when they get sick - surely we’re not using “people” medicine for animals, right? Wrong. In fact, farmers are more likely to use the inexpensive generic drugs that are less beneficial for human use due to increased resistance. This might not seem like a problem - if we can’t use them anyway, why not get some benefit? Sadly, some of these old medications are held in reserve to treat bacterial infections that are resistant to almost all antibiotics, but that were never exposed to these older drugs. As a result, using these “last line” drugs can create bacteria that are not only resistant to the drugs commonly used to treat infections, but also to these older drugs (7,8).
You’re wondering how, if sick animals can’t be sold, resistant bacteria transfer from healthy animals to people. There are a few ways, but nearly all of them are tied to food safety practices. The possibly grossest method is via feces: the animal passes stool, and water washes the resistant bacteria into a water source. This contaminated water is then used to water fresh vegetables that are likely not cooked before consumption. In fact, this is exactly how the Escherichia coli outbreak in 2006 occurred. A cattle farmer leased land to a spinach farmer, which became contaminated by infected cattle feces in the water supply. Because spinach is often consumed raw, the bacteria were able to reproduce without adequate control and without being eliminated when the food was cooked.
That last point - that the food wasn’t cooked - is the key to most of the remaining transferrals. Contaminated raw meats can spread bacteria to people as well. Meat that isn’t cooked to a temperature that kills the bacteria can lead to consumption of viable bacteria. This is why menus note that eating meat or eggs can cause problems in certain groups - undercooked eggs are another possible source of viable bacteria. But even if you’re careful to always cook your food to the right temperature, if you don’t cool it correctly and keep it out of the danger zone (4° - 60° Celsius), the bacteria can grow to a dangerous population after cooking. More than that, putting hot food into the refrigerator or freezer can raise the temperature of surrounding foods (including those that are pre-cooked) long enough to allow bacterial growth.
“Oh,” you say, “but I’m always careful to have my meat well done, my eggs over-hard, and to put leftovers away immediately without letting them heat surrounding food.” That’s awesome, but you’re not out of danger yet. There’s still cross-contamination to consider. This can occur if you cut or handle raw meat with the same hands or tools that you then use to handle fresh, uncooked food. This is why cutting boards for designated purposes have increased in popularity - keeping your raw chicken on one board, your red meat on another, your fruit and veg on yet another, helps reduce the risk of putting fruits and veggies into a pool left behind by raw meat. But if you don’t change your knife or wash your hands, you may still have cross contamination issues.
Cross-contamination can even occur before you bring your food home. If your meat and your fresh food aren’t stored correctly, the meat may contaminate the fresh food in your supermarket buggy or in your refrigerator. Meat stored above a crisper drawer may leak into the crisper drawer, especially if it isn’t wrapped well. Food put into the fridge without cleaning where the raw meat had been can then be infected as well. It’s also possible that food handlers (before it ever reached you) could be the cause of cross contamination.
Once you’ve consumed the contaminated food, the bacteria have the perfect host in which to grow and reproduce. As they grow, they interact with other bacteria in your body (remember the lesson in “Discussing the Disappearing Miracle”). The plasmids that contain the genes for resistance are then shared with bacteria present in your body, and now those bacteria are resistant to the drugs coming from the animal population.
Many have suggested that this sort of cross contamination between agricultural and human bacteria is incredibly unlikely. Sadly, a recent study in China (7,8) illustrates that resistant bacteria in animals are present in food and have caused disease in humans. Worse, the drug resistance is to a drug-of-last-resort. Colistin is an old antibiotic (developed in 1959), meaning it is now available in a generic formulation and thus cheap. It was also not widely used in humans due to the tendency to cause kidney problems, limiting the ability of bacteria common to humans to develop resistance to it. Because it is cheap, colistin has been widely used in agriculture, particularly in Asia, where it makes up 73.1% of colistin production. However, because so few things have had opportunity to develop resistance, infections that are resistant to other treatments are treated with colistin (when your choices are maybe develop kidney problems or die of the bacterial infection, medical professionals tend to opt for risking the kidney problems over death).
The study in China found colistin resistant bacteria in animals, raw meat in stores, and in 1% of hospital treated infections. Worse, this resistance has already spread from China and is now present in Malaysia. This means that patients are already seriously ill from antibiotic resistant infections that are also resistant to our last defense (7). We’re already seeing the first waves of a time when antibiotics may no longer be available. And while 1% may not seem alarming, remember that resistance spreads fast because bacteria share.
At the start of this article, I suggested that I would include information on how you, as an ordinary person, can help fight antibiotic resistance from agricultural use. I’ve already told you that safe food handling can help prevent the spread of bacteria to you and those you love, but that’s only one way to fight this growing threat. Many companies are already taking the steps necessary - Denmark (9) has outlawed the use of antibiotics in animals destined for market, and two turkey producers (10) have outlawed them either entirely or for subclinical usage. You can help make it more profitable for companies to take the longer road to growth by buying from trusted brands or demanding that your favorite brands eliminate subclinical use. You can demand better living conditions for animals bred for market - I didn’t even discuss how the terrible living conditions trigger preventative use of antibiotics or lead to sicker animals. The eggs that came from free-range hens are far less likely to have had antibiotics, because those hens are less likely to need them. But free-range hens require more land and more time and more food to grow, which increases the cost to the producer and the consumer.
Antibiotic resistance didn’t happen overnight. Many smart people are working on how to solve it, to keep our miracle intact for generations to come. Fixing a problem this big isn’t going to be easy or cheap. But you can help. You can demand that your food be antibiotic free, you can insist on only taking antibiotics when they’re actually necessary, and you can take every pill on time, to the end, even when you feel better (by the way, that’s actually a decent test to determine if your infection is viral or bacterial: viral infections last 7-10 days before the immune system can wipe them out. Bacterial infections treated by antibiotics will improve in a day or two. So if your doctors writes you a script for antibiotics, and you take them, and you aren’t better in a day or two, odds are your infection wasn’t bacterial. I give you permission to remind your doctor about the risks of antibiotic resistance). You can also educate others, like I did here. Understand the risks, do the hard work to help reduce them, and encourage others to do the same. Together, we might just be able to win.
NB: I included not only the sources I cited here, but also several that I used as I prepared this article. Watch for a video from “In A Nutshell” to explain this very topic, as well. It isn’t cited here, but it’s coming.
Sources:
- http://www.businessinsider.com/how-big-turkeys-were-then-and-now-2015-11
- http://www.motherjones.com/environment/2014/11/turkey-bigger-thanksgiving-butterball-antibiotics
- https://en.wikipedia.org/wiki/Wild_turkey
- https://en.wikipedia.org/wiki/Domesticated_turkey
- http://amrls.cvm.msu.edu/pharmacology/antimicrobial-usage-in-animals/non-therapuetic-use-of-antimicrobials-in-animals/use-of-antibiotics-in-animals-for-growth-promotion
- https://ods.od.nih.gov/factsheets/VitaminB12-HealthProfessional/
- http://phenomena.nationalgeographic.com/2015/11/21/mcr-gene-colistin/
- http://www.thelancet.com/journals/laninf/article/PIIS1473-3099(15)00424-7/abstract
- http://www.cdc.gov/drugresistance/threat-report-2013/
- https://consumermediallc.files.wordpress.com/2015/11/turkey_report_final.pdf
- http://www.tandfonline.com/doi/full/10.1080/03079450903505771
- https://www.avma.org/KB/Resources/FAQs/Pages/Antimicrobial-Use-and-Antimicrobial-Resistance-FAQs.aspx
- http://scienceblogs.com/aetiology/2014/05/28/what-is-the-harm-in-agricultural-use-antibiotics/